Gene Hackman’s Wife Died of Rare Virus Linked to 3 New Deaths in California
- Three people in a rural town in California have died this year from hantavirus, public health officials reported.
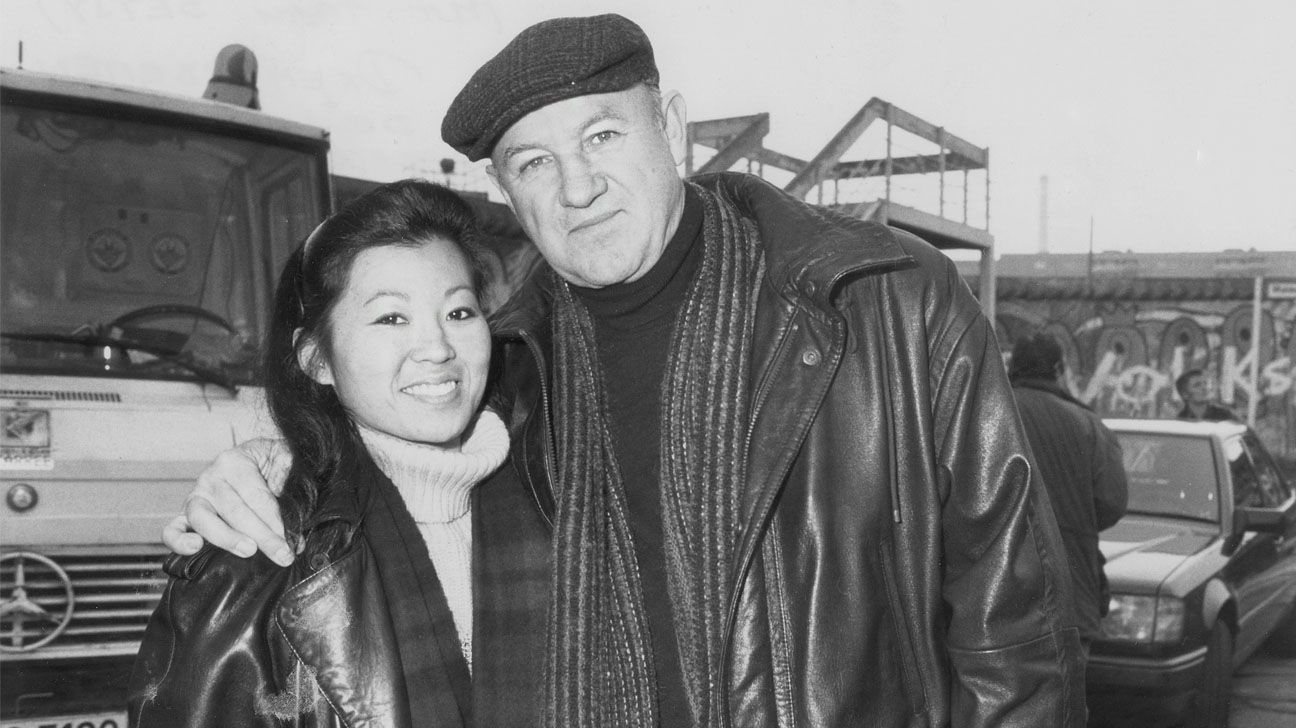
- The rare virus had killed actor Gene Hackman’s wife, Betsy Arakawa, in February. Hackman died a week later of heart disease with complications due to Alzheimer’s disease.
- Hantavirus is spread to people through droppings, urine, and saliva of infected rodents, mainly mice. It does not spread from person to person.
A rare virus that killed the wife of late actor Gene Hackman is linked to three deaths in the rural town of Mammoth Lakes, CA, state public health officials confirmed on April 3.
Hackman, 95, died of heart disease with complications due to Alzheimer’s disease about a week after his wife, Betsy Arakawa, 65, died of hantavirus pulmonary syndrome, the Associated Press reported. The partially mummified remains of the couple were found in their Santa Fe, NM, home on February 26.
Tom Boo, MD, a Mono County public health officer, called the situation in the rural town in the Eastern Sierra region “tragic and alarming” in a statement.
Hantavirus is a relatively rare virus that affects the lungs. People can become infected through the droppings, urine, or saliva of rodents, usually mice such as the deer mouse. The virus does not spread from person to person.
Michelle Harkins, MD, a pulmonologist with the University of New Mexico Health Sciences Center in Albuquerque, said it most commonly, but not always, occurs in rural areas.
“Exposure usually happens when people are cleaning out old sheds or going into mouse-infested areas around their property,” she told Healthline.
Sweeping up mouse droppings can cause the virus to become airborne, which people can then inhale, said Harkins. She has also seen patients who were exposed to the virus while working in the forest or on a construction site.
Deer mice are common in California’s Eastern Sierra region, but Boo said in the statement that their numbers are thought to be higher than typical this year. This could increase the risk of people being exposed to hantavirus.
While hantavirus can be potentially deadly, David Cutler, MD, a family medicine physician at Providence Saint John’s Health Center in Santa Monica, Calif., said it’s important to keep the risk of this virus in perspective.
“In the United States, where there’s generally good hygiene, and you don’t have a lot of people living in rural areas where rodent droppings are common, hantavirus is going to be very rare, but not impossible to contract,” he told Healthline.
Also, “there have been fewer than 1,000 cases of Hantavirus reported in the United States over the last 30 years,” he said. “In contrast, over 100,000 people die each year of viral infections that we can prevent, like COVID, flu and RSV.”
Cutler said it is just as important for healthcare workers, especially those who work in rural areas where hantavirus occurs, to be aware of this virus and its symptoms.
Symptoms of hantavirus
Cases of hantavirus are relatively rare, but they can be fatal. The Centers for Disease Control and Prevention reports that around one-third of people who develop lung-related symptoms die from the disease.
When the virus affects both the lungs and the cardiovascular system, about half of patients will die, said Harkins. In this phase, people can develop low blood pressure and fluid buildup in the lungs.
“Not everybody enters this cardiopulmonary phase, but a fair number do,” she said. “It can have a very rapid onset, and people can die within hours to a day or so without supportive care and monitoring.”
Early symptoms of hantavirus infection start to show one to eight weeks after exposure, said the CDC, and include:
- fatigue
- fever
- muscle aches
About half of people infected will also experience:
- headaches
- dizziness
- chills
- abdominal problems such as nausea, vomiting, diarrhea and abdominal pain
People may go on to develop respiratory symptoms such as:
- coughing
- shortness of breath
- tightness in the chest
Hantavirus cases appearing earlier than usual
The Centers for Disease Control and Prevention (CDC) reports that most cases of hantavirus occur west of the Mississippi River. The highest number is in New Mexico, followed by Colorado, Arizona, and California.
In the Eastern High Sierras, hantavirus cases typically occur later in the spring and in the summer, said Boo. So “the occurrence of three cases in a short period has me worried, especially this early in the year,” he added.
The early appearance of cases this year may be, in part, due to climate change.
“We know that there’s a cycle,” said Harkins. “Mild winters and summer rainfalls can increase the vegetation and the mouse population. When there are more mice around, they are more likely to become infected and spread the virus among themselves.”
None of the people who died in Mammoth Lakes had appeared to have engaged in high-exposure activities such as cleaning poorly ventilated indoor areas or other buildings with a lot of mouse waste, Boo said.
“Instead, these folks may have been exposed during normal daily activities, either in the home or the workplace,” he added.
Harkins said there are several things you can do to reduce your risk of exposure to hantavirus, such as:
- Rodent-proof your home by keeping doors and windows shut, sealing gaps in walls, and keeping outside wood piles away from the house.
- Air out enclosed areas for at least 30 minutes before entering if you see rodent droppings.
- Avoid vacuuming or sweeping rodent droppings, urine or nests, because this can cause the virus to become airborne.
- Spray droppings and contaminated areas with a disinfectant or 10% bleach solution and let it sit for five minutes before wiping the area.
- Wear gloves and an N-95 (or higher) mask while cleaning contaminated areas.
“If you do happen to go into a shed and clean it out, or you’re getting out Christmas decorations and there’s a mouse nest in the box, watch your symptoms afterward and seek medical care if you start to have symptoms,” said Harkin. “But keep in mind that this can be delayed by one to eight weeks after the initial exposure.”
Gene Hackman’s Wife Died of Rare Virus Linked to 3 New Deaths in California Read More »





